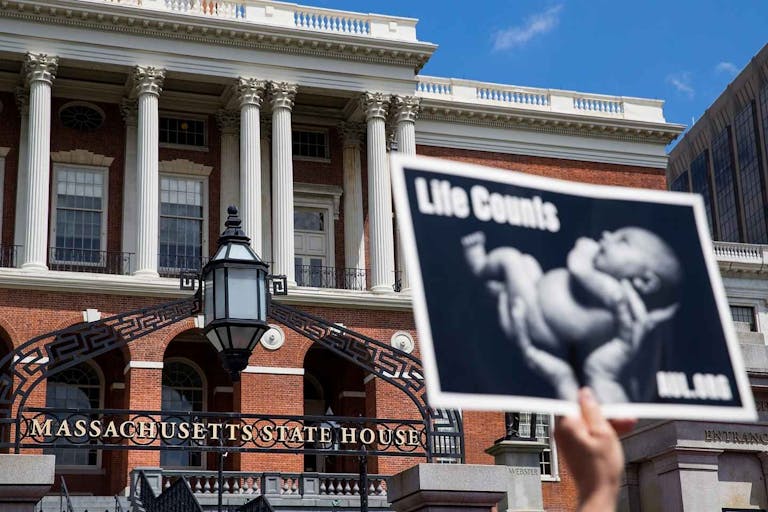
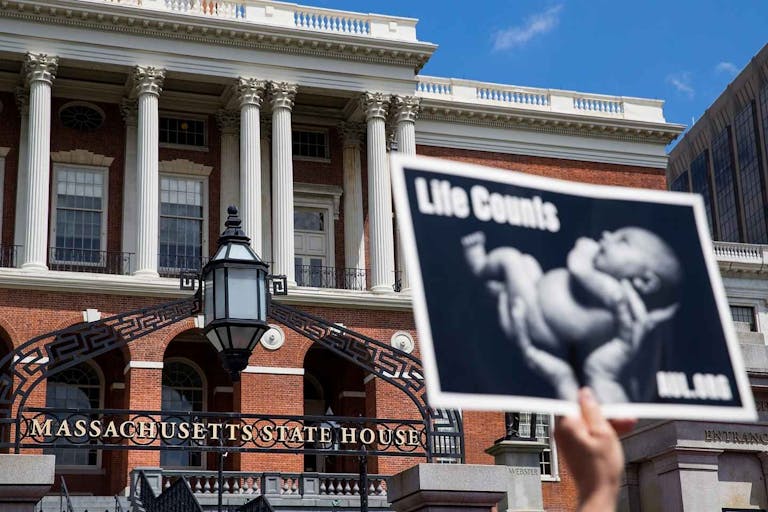
Massachusetts Health Department wants primary care to include abortion
Cassy Cooke
·
Fact Checks·By Anne Marie Williams, RN, BSN
Can IUDs kill human embryos before implantation? Here are the facts.
Many pro-life women seeking to prevent pregnancy may steer clear of oral contraceptives like the Pill, understanding that they can be abortifacient (potentially ending a child’s life by preventing implantation of the newly-created embryo). These women may pursue intrauterine device (IUD) placement instead, having heard that IUDs are contraceptive only. But is that true?
Let’s look at how IUDs are supposed to prevent conception— also known as their mechanism(s) of action— and then at the evidence that they can, or can’t, function as abortifacients.
How do IUDs act as contraception?
IUDs along with implants are considered long-acting reversible contraceptives (LARC), and their use is on the rise, despite an unsavory and not-so-distant past for IUDs in particular. IUDs are markedly different from oral contraceptives like the Pill because ovulation prevention is not their main mechanism of action, i.e. the main way they work. There are 2 types of IUDs, categorized by the main active ingredient.
Paragard Copper-IUD
Copper-IUDs are often called more “natural” because they continuously release copper into the uterus rather than hormones. Paragard is the only brand of copper-IUD sold in the U.S., and according to its full prescribing information, “Paragard works by preventing sperm from reaching the egg, preventing sperm from fertilizing the egg, or possibly preventing attachment (implantation) in the uterus. Paragard does not stop your ovaries from making an egg (ovulating) each month.”
Paragard is unlike the Pill, then, because it does not prevent ovulation, meaning that a mature egg could logically be available each cycle for potential fertilization by any sperm that the copper doesn’t kill or otherwise incapacitate. If fertilization occurs, the newly formed embryo would be unable to implant in the uterine lining or endometrium due to the hostile, inflammatory environment maintained by the continuous release of copper.
And indeed, a 2008 European Society of Human Reproduction and Embryology (ESHRE) workshop report notes, “It is very likely that the high degree of efficacy is related in part to the embryotoxic effect of high copper ion concentrations. The associated inflammatory changes also make the endometrium unfavourable for implantation (Stanford and Mikolajczyk, 2002).”
Mirena and other LNG-IUDs
The other type of IUD is hormonal and contains the progestin Levonorgestrel (LNG) as its main active ingredient. Mirena, Kyleena, and Skyla/Jaydess are all LNG-IUDs. As with copper-IUDs, LNG-IUDs don’t primarily work by stopping ovulation. According to Mirena manufacturer Bayer’s full prescribing information “Because the contraceptive effect of Mirena is mainly due to its local effects within the uterus, ovulatory cycles with follicular rupture usually occur in women of fertile age using Mirena… In a 1-year study, approximately 45% of menstrual cycles were ovulatory, and in another study after 4 years, 75% of cycles were ovulatory.”
How do Mirena and other IUDs work, then? The manufacturer doesn’t exactly know!
“The local mechanism by which continuously released LNG contributes to the contraceptive effectiveness of Mirena has not been conclusively demonstrated.” Potential mechanisms of action include “thickening of cervical mucus preventing passage of sperm into the uterus, inhibition of sperm capacitation or survival, and alteration of the endometrium.”
Both copper-IUDs and LNG-IUDs are considered highly effective at preventing pregnancy.
The FDA says of both copper-IUDs and LNG-IUDs, “Out of 100 women who use this method, less than 1 may get pregnant,” though a 2022 study published in the Journal of Internal Medicine found that in the first year after insertion, 2.4% of women with a LNG-IUD and 2.99% of women with a copper-IUD experienced an unplanned pregnancy. But if neither type of IUD consistently prevents ovulation, meaning that some fertilizations undoubtedly occur, what can account for their high rate of pregnancy prevention effectiveness?
How could IUDs be abortifacient?
Article continues below
Dear Reader,
Have you ever wanted to share the miracle of human development with little ones? Live Action is proud to present the "Baby Olivia" board book, which presents the content of Live Action's "Baby Olivia" fetal development video in a fun, new format. It's perfect for helping little minds understand the complex and beautiful process of human development in the womb.
Receive our brand new Baby Olivia board book when you give a one-time gift of $30 or more (or begin a new monthly gift of $15 or more).
From the mechanisms of action for both copper-IUDs and LNG-IUDs, which do not stop ovulation and which specifically mention prevention of implantation as a possible mechanism of action, the capacity of IUDs to cause early, preimplantation abortions is clear.
In 1972, thanks to the successful propagandistic efforts of abortion advocacy organizations, the American College of Obstetricians and Gynecologists (ACOG)— the professional organization for OB/GYNs and other women’s healthcare providers— arbitrarily redefined conception from occurring at fertilization to occurring at implantation of the embryo in the uterus.
By this erroneous new definition, prevention of implantation, which occurs 6-7 days after fertilization, would not constitute an abortion because conception hasn’t yet occurred. But fertilization—not implantation—marks the new existence of a genetically unique, separate individual.
If thickened cervical mucus from the LNG-IUD doesn’t prevent sperm from reaching a newly released egg, or similarly if the copper in a copper-IUD doesn’t incapacitate all the sperm and one does reach a newly released egg, fertilization can occur. But in either case, an early abortion would be expected due to inability to implant in the thinned lining of the uterus. Even this Huffington Post article admits that, when used as emergency contraception, copper-IUDs may be abortifacient “in a small number of cases.”
How often might IUDs act as abortifacients?
A 2020 literature review sought to answer this very question. The review authors found that most of the studies were old. Even the best studies were only of moderately good quality, and many were low quality, suggesting that this is a necessary area for further research.
The review authors also observed that research comparing rates of postfertilization but preimplantation pregnancy loss (also called early pregnancy loss or subclinical pregnancy loss, or a very early miscarriage) in women using IUDs versus in normally ovulating women not using any form of contraception (which would be considered spontaneous early miscarriage) is not available.
Nonetheless, previous research does offer some useful information regarding how often IUDs might be abortifacient and why truly accurate rates of loss are hard to come by.
While most studies of postfertilization, preimplantation pregnancy loss tested ꞵ-hCG (human chorionic gonadotropin, also known as the pregnancy hormone) levels, the literature review authors noted that these levels only rise after implantation. If a study only measures these levels, it can’t accurately assess rates of postfertilization but preimplantation pregnancy loss in IUD users. Even still, “Overall, with all women studied in all publications of any quality, 7.3 percent of IUD users had evidence of fertilization and pregnancy failure (see Table 3). With only good-quality studies included, 4.5 percent of IUD users had evidence of fertilization and pregnancy failure.”
Interestingly, another blood test called Hsp10 or early pregnancy factor “is more likely to detect the presence of early embryos that do not survive to implantation and the point of elaboration of detectable levels of β-hCG.” Hsp10 is a protein that helps the mother’s immune system accommodate her genetically foreign offspring, and it’s released long before ꞵ-hCG levels rise. In the one small study of Hsp10 that the authors found from 1992, researchers identified “the occurrence of fertilization with a probable failure of the fertilized ovum to implant in the endometrium of the uterus in 26 percent of the cycles studied.”
The 2008 ESHRE workshop report similarly concluded, “There is sufficient evidence to suggest that IUDs can prevent and disrupt implantation. The extent to which this interference contributes to its contraceptive action is unknown. The data are scanty and the political consequences of resolving this issue interfere with comprehensive research.”
Why isn’t the abortifacient capacity of IUDs more widely discussed?
Perhaps the best summary of why IUDs’ ability to act as abortifacients isn’t more widely discussed comes from the 2008 ESHRE workshop report, which tellingly noted:
… [I]f it was conclusively shown that [IUDs can] prevent the embryo from implanting, then [they] would be considered by the Roman Catholic church as causing an early abortion. As a result many agencies involved in the research, development or delivery of contraception prefer to leave the mechanism of action issue unresolved, which may explain why research into the contraceptive mechanisms of IUDs has been sparse in the last twenty years.
Live Action News is pro-life news and commentary from a pro-life perspective.
Contact editor@liveaction.org for questions, corrections, or if you are seeking permission to reprint any Live Action News content.
Guest Articles: To submit a guest article to Live Action News, email editor@liveaction.org with an attached Word document of 800-1000 words. Please also attach any photos relevant to your submission if applicable. If your submission is accepted for publication, you will be notified within three weeks. Guest articles are not compensated (see our Open License Agreement). Thank you for your interest in Live Action News!
Cassy Cooke
·
Fact Checks
Nancy Flanders
·
Fact Checks
Nancy Flanders
·
Fact Checks
Cassy Cooke
·
Fact Checks
Madison Evans
·
Fact Checks
Nancy Flanders
·
Human Interest
Anne Marie Williams, RN, BSN
·
Issues
Anne Marie Williams, RN, BSN
·
Analysis
Anne Marie Williams, RN, BSN
·
Analysis
Anne Marie Williams, RN, BSN
·
Issues
Anne Marie Williams, RN, BSN
·