Research shows Catholic support for IVF declines once Church teaching is understood
Angeline Tan
·
Did the NHS treat Iris poorly because she had Down syndrome?
People with disabilities in the United Kingdom have been speaking out against their society’s seemingly pervasive ableist attitude. Nowhere can this be seen more clearly than on the issue of abortion; in the United Kingdom, abortion is banned after 24 weeks of pregnancy… unless the baby has a disability of any kind, in which case parents are free to have an abortion. Even if the disability is easily correctable, like a cleft lip, parents can have a late-term abortion. And it’s not uncommon that parents who want to choose life for their preborn children find themselves pressured to kill them instead. This is the experience that Ben and Hannah Day had to suffer through after learning their preborn daughter, whom they named Iris, had Down syndrome. They fought for her life, but only a few months after she was born, Iris died. And the Days blame the NHS.
Iris was not diagnosed with Down syndrome until 36 weeks of pregnancy, meaning that she was almost completely full term. But the Days were pressured to have an abortion anyway. “From the outset, we felt like we were steered towards an abortion,” Ben said. Hannah added, “I just don’t agree with this notion that, if the baby’s not perfect, it shouldn’t be brought into the world. Because Iris was an IVF baby, for us she was our little miracle. She was so wanted – and every day with her was precious.”
Pressured to abort
The concern that Iris might have Down syndrome began during an ultrasound, where Iris was found to have Atrioventricular septal defect, or AVSD, a heart defect where there are several holes in the heart walls. It’s commonly found in children with Down syndrome, so Hannah had an amniocentesis performed. But first, they met with a maternal-fetal medicine specialist. “He said to us, ‘Can I ask what you will do if it’s confirmed that your baby has Down’s syndrome?’,” Hannah said. The couple was confused, and asked him to explain, so he asked, “Will you continue with the pregnancy?” Ben said of the conversation, “We were both taken aback. We didn’t even know abortion was an option. It was awful.” And while abortion was not explicitly mentioned, his point was clear. “What else could he have been suggesting, really?” Hannah asked. “We were offered a termination at 36 weeks, which is disgusting,” Ben said.
An abortion so late in term would most likely be an induction abortion, explained below by former abortionist, Dr. Anthony Levatino:

They told the doctor that abortion was out of the question, and then a few days later, the diagnosis was confirmed. When they met with the doctor again, his behavior didn’t get any better. “It was in this meeting that he said, ‘Your child will be mentally retarded’,” Hannah recalled. “The way the news was delivered was diabolical,” Ben said. I don’t know anyone who uses that word anymore.” They were given a pamphlet about Down syndrome, which Ben described as “abhorrent.” “It was a list as long as your arm saying, ‘These are the things that could be wrong with your child; these are the challenges you are going to face’,” Ben explained. “Basically, everything we heard from the NHS was very negative.”
Hannah said that, to her, the idea of having an abortion at 36 weeks was “inhumane.” “You’ve felt the baby kick, at this point you’ve had the nursery done – you are on the countdown to D-day,” she said.
According to an inquiry by Parliament into the issue of abortion and disability, parents who refuse abortion “are sometimes treated as selfish and irresponsible pariahs who foisted a disabled child upon society,” and can face “pressure or a feeling of disapproval from medical staff, as if they were doing wrong by bringing into the world a child who will require extra NHS resources.”
It’s this attitude that makes the couple question if NHS is responsible for Iris’s death.
Article continues below
Dear Reader,
In 2026, Live Action is heading straight where the battle is fiercest: college campuses.
We have a bold initiative to establish 100 Live Action campus chapters within the next year, and your partnership will make it a success!
Your support today will help train and equip young leaders, bring Live Action’s educational content into academic environments, host on-campus events and debates, and empower students to challenge the pro-abortion status quo with truth and compassion.
Invest in pro-life grassroots outreach and cultural formation with your DOUBLED year-end gift!
The long wait
After Iris was born, in June of 2016, she was referred to Evelina Children’s Hospital in London for heart surgery, which is recommended for children between three and six months old for AVSD. Research shows that the surgery should happen sooner rather than later. But according to the Days, “there was never any urgency,” and her surgery date was not scheduled until November, when Iris was over four months old. But three days before her scheduled surgery, Iris began to deteriorate. The Days took her to the emergency room at Colchester Hospital when she began to have breathing problems, a temperature, and a rash. Iris was treated for an infection, and then sent home. Her surgery was then pushed back, almost a month later. But then, the surgery was canceled again, because there was no bed available in the intensive care unit.
“I was getting quite angry,” Ben said. “We’d been told this operation needed to be done soon.” The surgery had now been pushed back another five days — only to get delayed again, because another child was supposedly sicker than Iris. “It was so upsetting, I could hardly speak,” Hannah said. Iris was discharged from the hospital the night before her surgery was supposed to take place, without being seen by a doctor, and without an ECG to make sure that her heart was not deteriorating. “This was an ill child, not a tin of beans,” Ben said. “It was ridiculous.”
The surgery was then pushed back to the beginning of December, but Iris would not survive to see it. When she had trouble breathing again, her parents took her back to Colchester Hospital. She seemed to improve, so doctors said that it was safe for Hannah and Ben to go home for a short while to get a break. But after they left, Iris began to deterioriate, fast. The Days rushed back to the hospital, but by the time they got there, it was too late. Iris had passed away.
It was later discovered that medical staff had neglected to notice warning signs about Iris’ condition, which should have prompted them to escalate her care sooner, and thus save her life. “We feel that the majority of NHS staff who came into contact with Iris in her short life let her and us down in the worst possible way,” they said. “As her parents, we were made to feel like an annoyance to the NHS on the day she died – and on every day after she was diagnosed with Down’s syndrome.”
A disturbing attitude
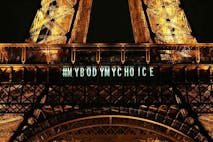
It’s not clear whether NHS staff intentionally gave Iris substandard care because she had Down syndrome. But it’s clear that this is another case showing the disturbing attitude towards disability in the United Kingdom, something that even British lawmakers have pointed out themselves. Lord Peter Shinkwin, who has brittle bone disease (or osteogenesis imperfect), has repeatedly spoken out against the legalization of late-term abortion for preborn children diagnosed with disabilities. According to Shinkwin, people with disabilities are “facing extinction” in the United Kingdom, so he has been working to change the law allowing babies with disabilities to be targeted for violent late-term abortions. But the problems run much deeper than just abortion being available.
A parliamentary commission found that parents of children diagnosed with disabilities prenatally are heavily pressured towards abortion, and — unsurprisingly — the number of abortions of children with disabilities is sharply rising. In 2015, an estimated 3,213 babies in the United Kingdom were aborted because they were diagnosed with a disability, marking a 68 percent increase over 10 years. As if this wasn’t bad enough, other British lawmakers have called for born children with disabilities to be “put down,” or forcibly aborted against their parents’ will.
Is it really a question, then, that people with disabilities like Iris might be at higher risk of receiving substandard medical care? The Days believe that if Iris had received the treatment she needed and deserved, she would still be alive today. And sadly, they very well might be right.
Live Action News is pro-life news and commentary from a pro-life perspective.
Contact editor@liveaction.org for questions, corrections, or if you are seeking permission to reprint any Live Action News content.
Guest Articles: To submit a guest article to Live Action News, email editor@liveaction.org with an attached Word document of 800-1000 words. Please also attach any photos relevant to your submission if applicable. If your submission is accepted for publication, you will be notified within three weeks. Guest articles are not compensated (see our Open License Agreement). Thank you for your interest in Live Action News!
Angeline Tan
·
International
Cassy Cooke
·
International
Angeline Tan
·
Politics
Stefano Gennarini, J.D. and Kelly Heilman, J.D.
·
Politics
Bridget Sielicki
·
Politics
Angeline Tan
·
International
Cassy Cooke
·
Analysis
Cassy Cooke
·
Analysis
Cassy Cooke
·
Analysis
Cassy Cooke
·
Analysis
Cassy Cooke
·