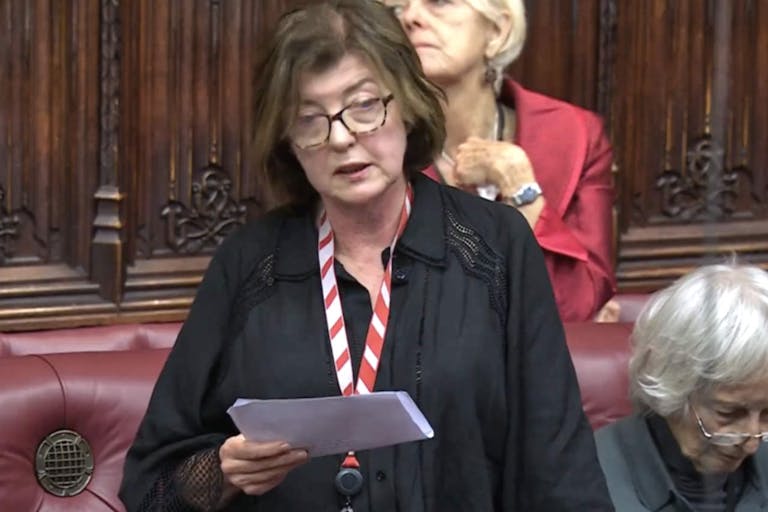
UK Prime Minister's former Chief of Staff slams assisted suicide bill
Right to Life UK
·
Analysis·By Anne Marie Williams, RN, BSN
New study shows double heart attack and stroke risks among healthy young contraceptive users
A Swedish study published on February 12, 2025, in the British Medical Journal found that current hormonal contraceptive use doubled — and even tripled — heart attack and stroke risk.
When researchers reviewed 25 years’ worth of medical records (1996-2021) from over 2,000,000 women, they found that the most popular forms of hormonal contraception except the progestin-only (Levonorgestrel-IUD or LNG-IUD) raised ischemic stroke risk, and all but the LNG-IUD and the arm patch raised heart attack (myocardial infarction) risk.
Ischemic (caused by a blood clot or other blockage in the brain) stroke risk was highest in arm patch users, with triple the rates compared to women who did not use hormonal contraception. Vaginal ring and oral combined contraceptive (containing both estrogen and progestin) users had more than twice the stroke risk of non-users. Progestin-only pill users had lower risk than the other methods, but stroke rates were still significantly higher than in non-users.
Oral contraceptive users also had twice the heart attack risk compared to women who didn’t use hormonal birth control. Vaginal ring users had triple the heart attack risk. Progestin-only pill users were also at higher risk than non-users.
Let’s put the concept of double or triple the risk into context. As an example, the researchers noted that for oral contraceptive users, “[The increased risks] equate to approximately one extra ischemic stroke for every 4760 women using combined oral contraceptives for one year and one extra myocardial infarction for every 10,000 women per year of use compared with no users.”
Many wonder, and various commentaries ask in so many words, Why get excited about such small increases in risk? A Medscape commentary went so far as to explicitly proclaim, “Women should not stop using contraception based on the findings.” The headline of a LiveScience writeup of the BMJ study read, “Hormonal birth control may double risk of stroke, study finds — but don’t panic.”
The rub is that 248 million women worldwide use hormonal contraception. Calculating based on oral contraceptive usage statistics from the Centers for Disease Control and Prevention (CDC), between 2015 and 2017, over 9 million reproductive-aged American women were on combined contraceptive pills alone. Over 2 million women were using the contraceptive arm patch, vaginal ring, or Depo-Provera arm injection.
“Just” one extra ischemic stroke for every 4,760 women taking the pill for 12 months would translate to 1,890 contraceptive-caused ischemic strokes that year. And while risk does not appear to increase with duration of use (risk doesn’t go up for every additional year you’re on hormonal contraception), the fact remains that many women are exposed to these same risks year after year, because contraceptives are often used for years on end.
Furthermore, while side effects are bound to occur with any medication, those risks are outweighed or judged acceptable for the greater goal of improving symptoms or curing a disease.
But hormonal contraception is often taken for pregnancy prevention by healthy young women. When her birth control causes a stroke or heart attack or other serious complication like a blood clot, a healthy young woman is made ill by her contraceptive.
READ: ‘No adverse outcomes’ of hormonal contraception use? Not so fast, says expert panel
Article continues below
Dear Reader,
In 2026, Live Action is heading straight where the battle is fiercest: college campuses.
We have a bold initiative to establish 100 Live Action campus chapters within the next year, and your partnership will make it a success!
Your support today will help train and equip young leaders, bring Live Action’s educational content into academic environments, host on-campus events and debates, and empower students to challenge the pro-abortion status quo with truth and compassion.
Invest in pro-life grassroots outreach and cultural formation with your DOUBLED year-end gift!
Hormonal birth control apologists routinely point out that pregnancy and the early postpartum period bring heightened risk of blood clots, equivalent to or slightly higher than risk from hormonal contraceptives. Similarly, in a Medscape writeup of the BMJ study, a UK-based medical school professor was quoted as saying, “The risk of stroke and heart attack in pregnancy and postnatal period is significantly higher than the risks reported in this study for contraceptives.”
Live Action News previously put increased blood clot risk during pregnancy and postpartum vs. on hormonal contraceptives in context at length, explaining why it’s an apples to oranges comparison. The same logic holds for comparing stroke and heart attack risk in hormonal contraceptive users to pregnant and postpartum women.
Yes, heart attacks and strokes can occur in healthy pregnant and postpartum women, though they primarily occur in pregnant or postpartum women who are older, smoke, and/or have preexisting conditions such as high blood pressure, obesity, high cholesterol, and diabetes.
But consider that the average woman, who bears approximately two children, will experience higher clot risk for roughly two years, counting 2x 40 weeks of pregnancy plus 2x six weeks postpartum. By contrast, the average woman takes hormonal contraception off and on for much of her adult life, spanning decades of exposure to blood clot, heart attack, and stroke risk, to name a few.
According to a 2021 Guttmacher fact sheet, in order to achieve her desired family size, “a sexually active woman must use contraceptives for roughly three decades” (emphasis added).
Furthermore, while pregnancy has some surprising health benefits, hormonal contraception cannot resolve reproductive health issues; it can only serve as a sort of Band-Aid for them. Unfortunately, this distinction is rarely made in commentaries on studies of the risks of hormonal contraception.
Dr Oliver Segal, a British cardiologist and electrophysiologist, told Women’s Health UK, “The small increased risk of stroke or heart attack must be weighed against the benefits of hormonal contraception, including pregnancy prevention, menstrual cycle regulation and treatment of conditions such as polycystic ovary syndrome (PCOS) or endometriosis.”
Commentaries like the Medscape and Women’s Health UK articles imply that hormonal contraception is a panacea for virtually any women’s health condition, and indeed it’s been framed that way for decades. But healthcare providers trained in restorative reproductive medicine (RRM) seek to address the root causes of hormonal and other reproductive health disorders.
Rather than masking symptoms with hormonal contraception — which may contribute to, for example, the average 8-12 year delay between endometriosis symptom onset and diagnosis — they recognize that the menstrual cycle is a fifth vital sign of health. Cycle charting serves as the starting point for a thorough workup that may involve blood draws, ultrasounds, and more to get to the source and resolve underlying issues.
Women deserve family planning options and reproductive health solutions that don’t put their health at risk. Hormonal birth control cannot offer them that. It’s no wonder young women are increasingly realizing hormonal contraception’s limitations and seeking alternative options.
Live Action News is pro-life news and commentary from a pro-life perspective.
Contact editor@liveaction.org for questions, corrections, or if you are seeking permission to reprint any Live Action News content.
Guest Articles: To submit a guest article to Live Action News, email editor@liveaction.org with an attached Word document of 800-1000 words. Please also attach any photos relevant to your submission if applicable. If your submission is accepted for publication, you will be notified within three weeks. Guest articles are not compensated (see our Open License Agreement). Thank you for your interest in Live Action News!
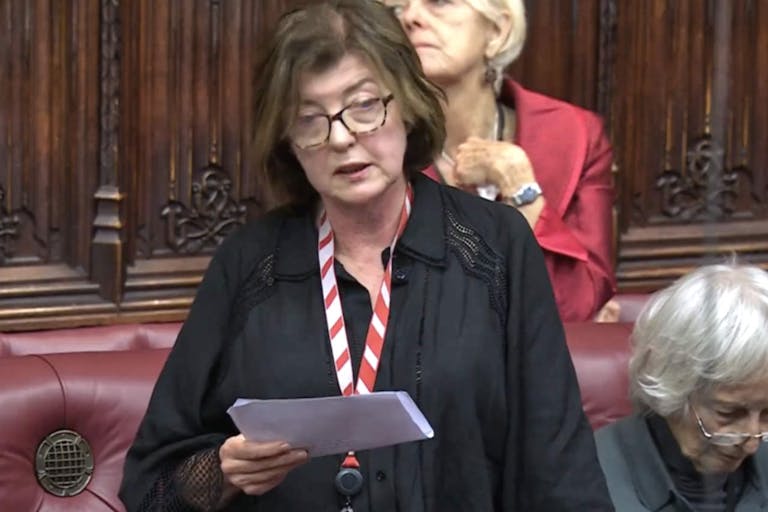
Right to Life UK
·
Pop Culture
Cassy Cooke
·
International
Cassy Cooke
·
Analysis
Cassy Cooke
·
Analysis
Angeline Tan
·
Analysis
Cassy Cooke
·
Human Interest
Anne Marie Williams, RN, BSN
·
Issues
Anne Marie Williams, RN, BSN
·
Analysis
Anne Marie Williams, RN, BSN
·
Analysis
Anne Marie Williams, RN, BSN
·
Issues
Anne Marie Williams, RN, BSN
·